Ever wondered how that "45cc" prostate volume on your radiology report was calculated? Behind every measurement lies a precise technique developed over decades. Understanding how radiologists measure your prostate helps you interpret results and have informed conversations with your healthcare team.
Whether performed via transrectal ultrasound (TRUS) or MRI, prostate volume measurement follows standardized protocols. This guide takes you inside the radiology suite to understand exactly how these critical measurements are obtained.
The Imaging Modalities
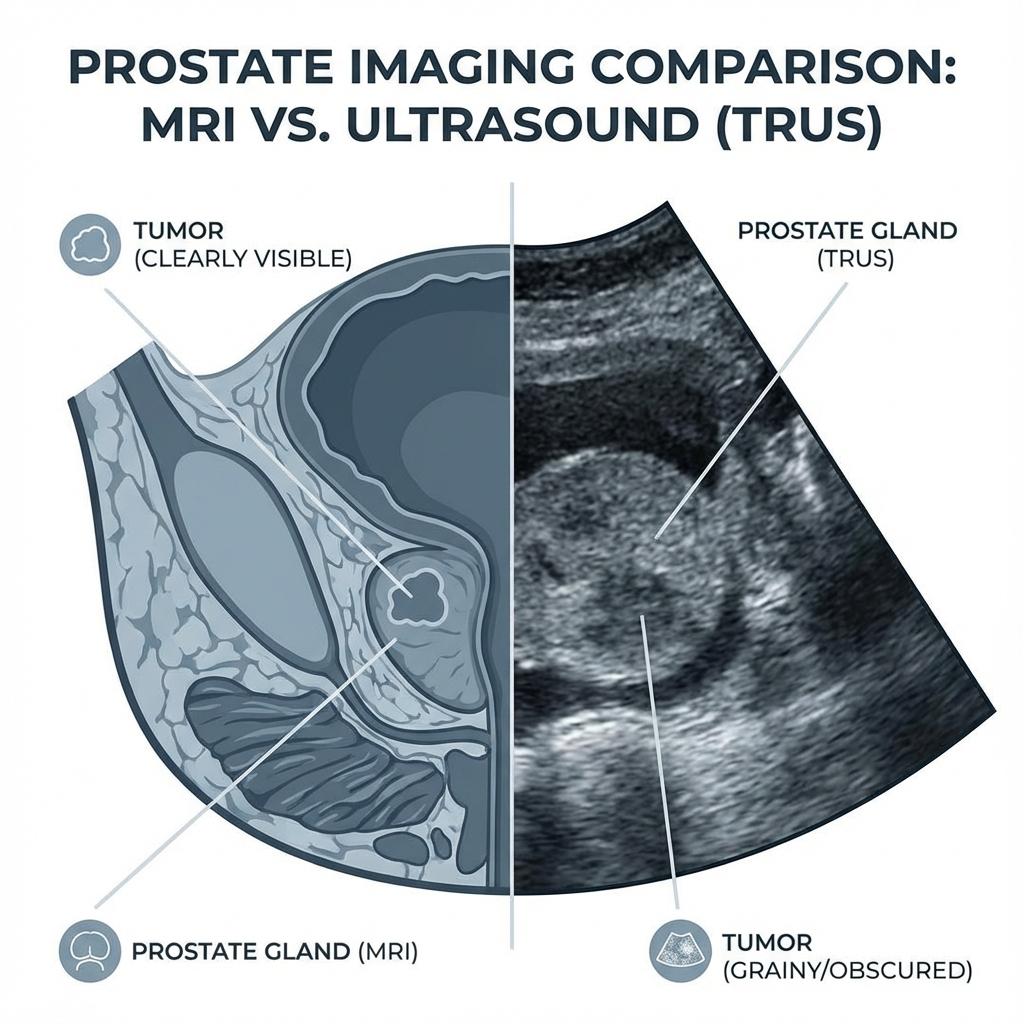
Transrectal Ultrasound (TRUS)
TRUS remains the most common method for prostate volume measurement due to its accessibility, low cost, and real-time imaging capability.
The Procedure:
- Patient lies on side with knees bent
- A lubricated ultrasound probe (about the size of a finger) is inserted into the rectum
- The probe emits high-frequency sound waves that create images
- Measurements are taken in multiple planes
TRUS offers resolution of approximately 0.5-1mm, sufficient for accurate dimensional measurements. The entire procedure takes 10-15 minutes.
Magnetic Resonance Imaging (MRI)
MRI provides superior soft tissue contrast and is increasingly used for prostate evaluation, especially when cancer is a concern.
- Multiparametric MRI (mpMRI): Combines multiple sequences for comprehensive evaluation
- Endorectal Coil (optional): Inserted for higher resolution images
- Acquisition Time: 30-45 minutes for full protocol
For a detailed comparison, see our TRUS vs MRI accuracy analysis.
The Three Essential Measurements
Regardless of imaging modality, radiologists measure three dimensions that approximate the prostate as an ellipsoid:
1. Transverse (Width) Diameter
- Measured on: Axial (cross-sectional) plane
- Landmarks: Maximum width of gland, typically at mid-gland level
- Typical range: 3.5-5.5 cm
- Technical note: Measured perpendicular to the urethra
2. Anterior-Posterior (AP/Depth) Diameter
- Measured on: Axial or sagittal plane
- Landmarks: From anterior capsule to posterior capsule at mid-gland
- Typical range: 2.5-4.5 cm
- Common error: Including periprostatic fat or seminal vesicles
3. Craniocaudal (Height/Length) Diameter
- Measured on: Sagittal or coronal plane
- Landmarks: From apex (near urethral sphincter) to base (near bladder)
- Typical range: 3.0-5.0 cm
- Challenge: Apex can be difficult to delineate
Terminology Note
Radiology reports may use "length" interchangeably with AP diameter or craniocaudal length. Always check the measurement plane to know which dimension is which.
The Measurement Technique
Step 1: Image Acquisition
The radiologist or sonographer acquires images in multiple planes:
- Sagittal: Side view, showing length from base to apex
- Axial/Transverse: Cross-section, showing width and AP diameter
- Coronal: Front view (mainly for MRI)
Step 2: Identify Anatomic Landmarks
Proper measurement requires identifying:
- The prostatic capsule (outer boundary)
- The verumontanum (landmark for mid-gland)
- The bladder base (superior boundary)
- The urogenital diaphragm (inferior boundary/apex)
Step 3: Place Calipers
Electronic calipers are placed at the edges of the prostate in each dimension. Most modern systems can calculate volume automatically once three measurements are entered.
Step 4: Apply the Formula
The standard Ellipsoid formula is applied:
Volume = W × AP × L × 0.52
Our Prostate Volume Calculator uses this same formula. You can verify your radiologist's calculation by entering your dimensions.
Sources of Measurement Error
No measurement is perfect. Understanding error sources helps interpret results:
Operator Variability
Studies show inter-observer variability of 10-20% even among experienced radiologists. Two radiologists measuring the same images may report different volumes.
Plane Selection
Oblique imaging planes can distort measurements. True axial/sagittal/coronal alignment is essential.
Boundary Definition
The prostatic capsule can be indistinct, especially in areas of BPH nodularity or at the apex. This "edge effect" affects measurement precision.
Shape Assumptions
The Ellipsoid formula assumes a symmetric shape. Irregular prostates (median lobe, asymmetric BPH) may not fit this model well. Learn more in our formula comparison article.
Imaging Limitations
- TRUS: Limited by acoustic shadowing from calcifications
- MRI: Motion artifact, breathing, intestinal gas can degrade images
Advanced Techniques
Planimetric Volumetry (MRI)
For maximum accuracy, radiologists can trace the prostate outline on every MRI slice and sum the areas. This "planimetry" method is within 5% of true volume but is time-consuming.
3D Ultrasound
Newer 3D TRUS systems acquire volumetric data and can:
- Reduce operator dependency
- Enable multiplanar reconstruction
- Provide semi-automated segmentation
AI-Assisted Measurement
Machine learning algorithms are being developed to automatically segment the prostate on MRI, potentially reducing variability and measurement time.
Quality Assurance
How do radiology departments ensure accurate measurements?
- Standardized Protocols: Written procedures for probe placement and measurement technique
- Case Conferences: Reviewing discrepant measurements
- Phantom Studies: Measuring objects of known volume to verify equipment accuracy
- Correlation Studies: Comparing imaging volumes to surgical specimen weights
Why Measurement Accuracy Matters
A 20% measurement error translates to real clinical consequences:
PSA Density Interpretation
If true volume is 50cc but reported as 40cc, PSA Density appears 25% higher—potentially triggering an unnecessary biopsy. See our PSA Density guide.
Treatment Eligibility
Some procedures have strict volume cutoffs (e.g., UroLift: 30-80cc). Measurement error could incorrectly include or exclude patients.
Surgical Planning
Estimating blood loss and procedure duration depends on accurate volume. Our Prostate Weight Calculator can help with surgical planning.
What Patients Should Know
Request Your Measurements
Ask for the three dimensions (not just the calculated volume) so you can verify the calculation yourself using our calculator.
Consistency Matters
When tracking volume over time, try to have measurements done at the same facility using the same modality. TRUS-to-MRI comparisons can show apparent volume changes that are actually just technique differences.
Understand the Margin of Error
Don't panic if your prostate "grew" from 42cc to 48cc between scans. This 14% change could be within measurement variability. Trends over multiple measurements are more reliable.
Key Takeaways
- ✓ Radiologists measure 3 dimensions: width, AP depth, and craniocaudal length
- ✓ These are combined using the Ellipsoid formula (W × AP × L × 0.52)
- ✓ Inter-observer variability of 10-20% is normal
- ✓ MRI planimetry is most accurate but time-consuming
- ✓ Consistent imaging protocols reduce measurement variability
Verify your radiology report dimensions with our free Prostate Volume Calculator to ensure the math adds up correctly.
Need to calculate prostate volume?
Use our free medical-grade calculator to get instant results using the Ellipsoid or Bullet formula.