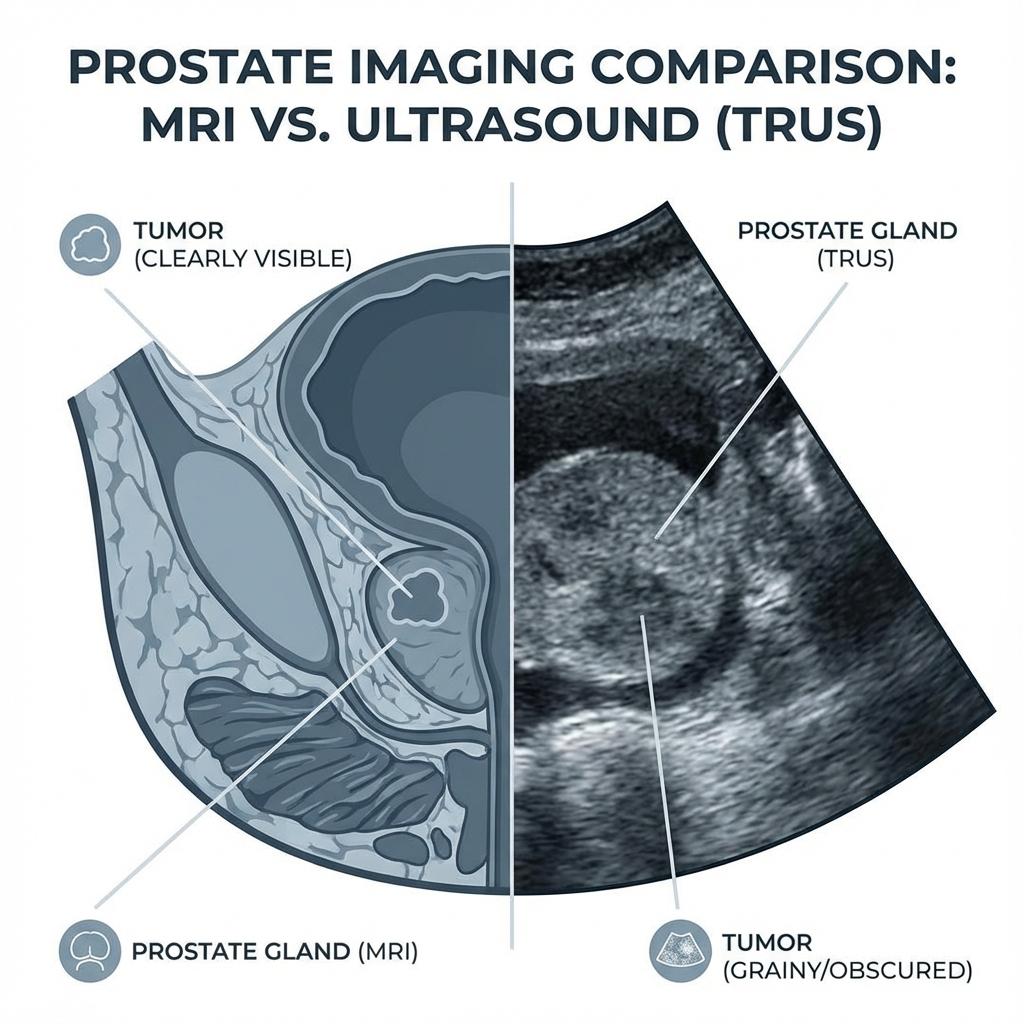
Accurate prostate volume measurement is the cornerstone of diagnosing Benign Prostatic Hyperplasia (BPH), assessing prostate cancer risk, and planning treatments. For decades, Transrectal Ultrasound (TRUS) has been the gold standard due to its accessibility and low cost. However, the rise of Multiparametric MRI (mpMRI) has challenged this dominance, offering superior resolution and anatomical detail.
The question remains: Which method is truly more accurate? And more importantly, does the difference in accuracy matter for your specific clinical situation? In this comprehensive guide, we analyze the technological differences, review the latest clinical studies, and explain why the method of measurement can drastically alter your diagnosis.
The Basics: How Each Method Works
1. Transrectal Ultrasound (TRUS)
TRUS has been the workhorse of urology since the 1980s. It involves inserting a slender ultrasound probe into the rectum. The probe emits high-frequency sound waves that bounce off the prostate gland, creating a real-time 2D image.
- The Procedure: It is typically performed in a urologist's office, often as part of a biopsy or a standalone measurement. It takes only a few minutes.
- Volume Calculation: Since the ultrasound provides a 2D cross-section, the urologist measures three dimensions: Length (L), Width (W), and Height (H). These are plugged into the Ellipsoid Formula (Volume = L × W × H × 0.52).
- Limitations: The "view" is limited by the rectum wall. Large prostates (over 80-100cc) are often harder to visualize completely, leading to "cutoff" errors where the edges of the gland are missed.
2. Multiparametric MRI (mpMRI)
Multiparametric MRI uses powerful magnetic fields and radio waves to create highly detailed cross-sectional images of the prostate. Unlike standard MRI, "multiparametric" means it combines different types of scans (T2-weighted, Diffusion-Weighted Imaging, etc.) to look at tissue density and blood flow.
- The Procedure: Requires the patient to lie still in an MRI machine for 30-45 minutes. It is non-invasive (no probe in the rectum) but can be claustrophobic for some.
- Volume Calculation: Radiologists can use the same ellipsoid formula as TRUS. However, modern software allows for Planimetry (or segmentation), where the outline of the prostate is traced on every single 3mm slice, and the volume is calculated by summing these areas. This method is mathematically far more precise.
The Accuracy Gap: What the Data Shows
The true test of accuracy is comparing the imaging measurement to the "radical prostatectomy specimen weight"—the actual weight of the prostate after it has been surgically removed.
The "Underestimation" Phenomenon
A systematic review of urological literature reveals a consistent trend: TRUS tends to underestimate prostate volume compared to the actual surgical weight.
Key Study Findings
- Study A (Journal of Urology): In 500 patients, TRUS underestimated volume by an average of 18%. MRI using the ellipsoid formula underestimated by 7%. MRI using planimetry was accurate within 3%.
- Study B (BJU International): Found that the error rate for TRUS increases as the prostate gets larger. For prostates >80cc, TRUS underestimation reached nearly 25%.
- Shape Matters: The Ellipsoid formula assumes the prostate is shaped like an egg. However, enlarged prostates (BPH) often grow asymmetrically, sometimes resembling a sphere or a flattened cylinder. The formula (L x W x H x 0.52) fails to capture this volume, whereas MRI planimetry accounts for every contour.
Why Does Accurate Volume Matter?
You might ask, "Does it matter if my prostate is 50cc or 60cc?" In many cases, yes. The volume is a critical denominator in several diagnostic ratios.
2. BPH Treatment Eligibility
Minimally Invasive Surgical Therapies (MISTs) often have strict volume criteria for safety and efficacy.
- UroLift: Generally indicated for prostates <80cc (some guidelines say <100cc). If TRUS incorrectly measures a 90cc prostate as 75cc, the patient might undergo a procedure that is doomed to fail.
- Rezum (Steam Therapy): Also has volume considerations.
- PAE (Prostate Artery Embolization): Often works better for very large glands. Knowing the true volume helps steer the patient toward PAE rather than TURP.
3. Active Surveillance Monitoring
For men with low-grade prostate cancer on active surveillance, "PSA Velocity" (rate of rise) is monitored. However, if the prostate is growing benignly, PSA will rise naturally. distinguishing "benign PSA rise" from "cancer progression" requires knowing the precise growth rate of the gland volume. MRI provides a much more reliable baseline for this year-over-year tracking.
Pros and Cons Summary
| Feature | TRUS | MRI (mpMRI) |
|---|---|---|
| Accuracy | Standard (good for screening) | Superior (Gold Standard) |
| Cost | Low ($) | High ($$$) |
| Availability | Every urology office | Imaging centers / Hospitals |
| Best For | Initial screening, Biopsy guidance | Pre-biopsy planning, Density calc, large glands |
| Invasiveness | High (Rectal probe) | Non-invasive (External) |
Which One Should You Trust?
If you have undergone both tests and the results are discrepant, trust the MRI—provided it was read by an experienced radiologist. The physics of MRI allow for a true 3D volumetric assessment that is simply not possible with a 2D ultrasound probe.
Advice for Patients:
- If your TRUS volume seems "small" but your PSA is high, ask for an MRI to confirm the density.
- If you are considering UroLift or Rezum, ensure your volume is measured recently, ideally by the modality that the surgeon trusts most.
- When tracking PSA Density over years, try to use the same imaging method consistently. Comparing a 2023 TRUS volume to a 2025 MRI volume will likely show "growth" that is actually just the difference in measurement accuracy.
Conclusion
TRUS remains a vital, cost-effective tool for everyday urology. However, it has a known tendency to underestimate prostate size, particularly in men with significant BPH. Multiparametric MRI offers a higher degree of precision.
In the era of precision medicine, knowing exactly how big your prostate is can be the difference between active surveillance and invasive treatment. Always ask your doctor which method was used and consider the "margin of error" when making life-changing health decisions.
Need to calculate prostate volume?
Use our free medical-grade calculator to get instant results using the Ellipsoid or Bullet formula.