The International Prostate Symptom Score (IPSS) is the most widely used questionnaire for assessing lower urinary tract symptoms in men. But what do those 7 questions actually measure? Understanding the science behind each question helps you answer accurately and get the most value from your results.
Originally developed as the American Urological Association Symptom Index (AUA-SI), the IPSS has been translated into over 50 languages and validated across diverse populations. Take our interactive IPSS Quiz to calculate your own score, then use this guide to understand what each answer means.
The Structure of the IPSS
The IPSS consists of 7 symptom questions plus 1 quality of life question:
- Questions 1-7: Scored 0-5 each (total: 0-35)
- Question 8: Quality of life (not included in total score)
Each symptom question asks how often you've experienced that particular problem over the past month, with answers ranging from "Not at all" (0) to "Almost always" (5).
Question 1: Incomplete Emptying
"Over the past month, how often have you had the sensation of not emptying your bladder completely after you finished urinating?"
What It Measures
This question assesses post-void residual sensation—the feeling that urine remains in your bladder even after you've finished urinating. Medically, this is called "sense of incomplete evacuation."
Clinical Significance
Incomplete emptying can indicate:
- Bladder outlet obstruction from enlarged prostate
- Weak detrusor (bladder muscle) contraction
- Urethral stricture
High scores here often correlate with measurable post-void residual (PVR)—the volume of urine left in the bladder after voiding, measured by ultrasound or catheterization.
When It's Most Troublesome
Men who score high on this question often describe needing to urinate again shortly after leaving the bathroom, or feeling like they're "never quite done."
Question 2: Frequency
"Over the past month, how often have you had to urinate again less than two hours after you finished urinating?"
What It Measures
This question quantifies urinary frequency—how often you need to urinate during waking hours. The two-hour threshold distinguishes abnormal frequency from normal hydration-related urination.
Clinical Significance
Urinary frequency can result from:
- Reduced bladder capacity (from BPH compression)
- Overactive bladder muscle
- Incomplete emptying (triggering another void soon after)
- High fluid intake (rule this out first!)
Practical Impact
Frequent urination disrupts work, travel, and social activities. Men with high scores here often plan activities around bathroom access.
Question 3: Intermittency
"Over the past month, how often have you found you stopped and started again several times when you urinated?"
What It Measures
Intermittency refers to a stop-and-start urinary stream. Instead of continuous flow, urine comes out in fits and starts.
Clinical Significance
Intermittency typically indicates:
- Obstruction at the bladder neck or prostate
- Detrusor muscle fatigue during voiding
- Coordination problems between bladder and sphincter
This symptom is highly specific to obstructive pathology—it rarely occurs without some degree of bladder outlet obstruction.
Question 4: Urgency
"Over the past month, how often have you found it difficult to postpone urination?"
What It Measures
Urgency is the sudden, compelling need to urinate that's difficult to defer. It's distinct from the gradual buildup of needing to go—urgency hits you suddenly.
Clinical Significance
Urgency is a key feature of overactive bladder (OAB), which often coexists with BPH. It can also indicate:
- Bladder irritation or infection
- Detrusor overactivity
- Incomplete emptying leading to constant "fullness"
Treatment Implications
High urgency scores may indicate need for anticholinergic or beta-3 agonist medications in addition to standard BPH treatment.
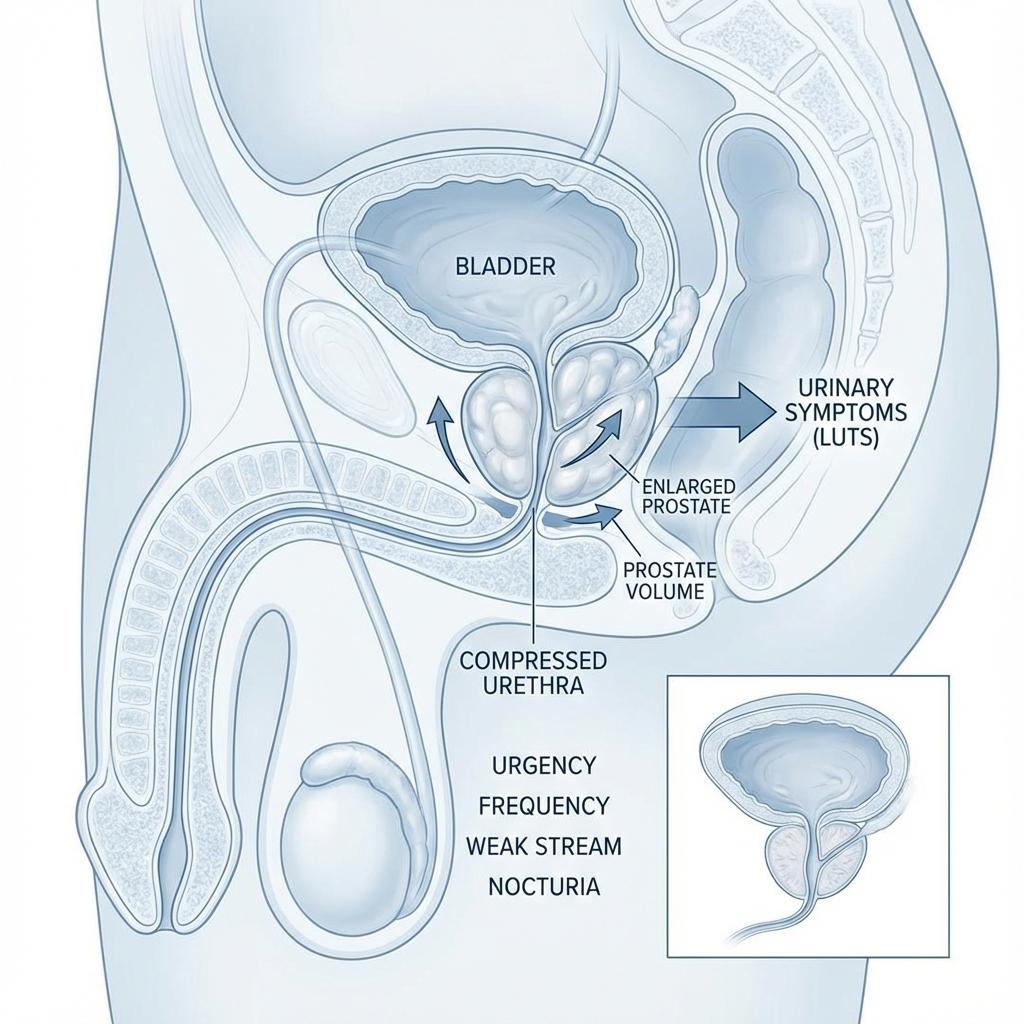
Question 5: Weak Stream
"Over the past month, how often have you had a weak urinary stream?"
What It Measures
This question assesses the force of the urinary stream. Men often describe this as "not peeing like I used to" or needing to stand closer to the toilet.
Clinical Significance
Weak stream is the classic obstructive symptom:
- Directly correlates with prostatic obstruction
- Can be objectively measured by uroflowmetry (max flow rate)
- Often improves most dramatically with BPH treatment
This symptom has the strongest correlation with prostate volume among all IPSS questions. Learn more about the relationship in our Volume-LUTS Connection article.
Question 6: Straining
"Over the past month, how often have you had to push or strain to begin urination?"
What It Measures
Straining refers to the need to use abdominal muscles to initiate or maintain urine flow. Normal voiding should be effortless—the bladder muscle does the work.
Clinical Significance
The need to strain indicates:
- Significant bladder outlet obstruction
- Possible detrusor weakness (the bladder can't overcome resistance)
- Risk for developing urinary retention
Warning Signs
Severe straining can lead to complications:
- Hernia development
- Hemorrhoid flare-ups
- Syncope (fainting) from vagal response
Question 7: Nocturia
"Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?"
What It Measures
Nocturia—nighttime urination—is scored differently:
- 0 = None
- 1 = One time
- 2 = Two times
- 3 = Three times
- 4 = Four times
- 5 = Five or more times
Clinical Significance
Nocturia is the most bothersome symptom for many men because it disrupts sleep. However, its causes are complex:
- BPH-related: Incomplete emptying, reduced bladder capacity
- Non-prostatic: Nocturnal polyuria, heart failure, sleep apnea, diabetes
Because of this complexity, nocturia often doesn't fully resolve with prostate treatment alone.
Quality of Life Question
"If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that?"
This question (scored 0-6) isn't included in the symptom total but is clinically crucial. A man with mild symptoms (IPSS 8) who's "terribly unhappy" may warrant treatment, while one with moderate symptoms (IPSS 18) who's "mostly satisfied" may prefer watchful waiting.
Interpreting Your Total Score
After completing all 7 symptom questions, scores are categorized:
| Score Range | Severity | Typical Management |
|---|---|---|
| 0-7 | Mild | Watchful waiting, lifestyle changes |
| 8-19 | Moderate | Medication therapy; consider intervention if QoL impacted |
| 20-35 | Severe | Active treatment usually indicated; surgical options discussed |
Key Takeaways
- ✓ The IPSS measures 7 specific symptoms: emptying, frequency, intermittency, urgency, weak stream, straining, nocturia
- ✓ Each question targets a different aspect of lower urinary tract dysfunction
- ✓ Scores 0-7 = Mild, 8-19 = Moderate, 20-35 = Severe
- ✓ Quality of life matters as much as symptom severity for treatment decisions
- ✓ Tracking your IPSS over time shows treatment response
Ready to calculate your IPSS? Take our free IPSS Symptom Score Quiz to get your score with detailed interpretation.
Need to calculate prostate volume?
Use our free medical-grade calculator to get instant results using the Ellipsoid or Bullet formula.